What Is Intermittent Fasting and How Does It Work?
Common intermittent fasting methods and their eating/fasting windows
Intermittent fasting (IF) is not a diet but rather an eating pattern that cycles between periods of fasting and eating. Unlike traditional diets that focus on what to eat, intermittent fasting centres on when to eat. This approach has ancient roots in human evolution and various religious practices, but has recently gained scientific attention for its potential health benefits.
Common Intermittent Fasting Methods
- The 16/8 Method: Restricting eating to an 8-hour window daily while fasting for 16 hours
- The 5:2 Diet: Eating normally five days a week while limiting calories to 500-600 on two non-consecutive days
- Eat-Stop-Eat: Incorporating one or two 24-hour fasts per week
- Alternate-Day Fasting: Alternating between normal eating days and fasting or very low-calorie days
Primary Health Goals of Intermittent Fasting
People adopt intermittent fasting for various health objectives, including:
- Weight management and fat loss
- Improved insulin sensitivity
- Reduced inflammation
- Enhanced cellular repair (autophagy)
- Better heart health markers
- Potential longevity benefits
- Simplified meal planning
- Metabolic health improvements
When you fast, your body undergoes several metabolic changes. After depleting glucose stores (typically within 8-12 hours of fasting), your body shifts to burning stored fat for energy. This metabolic switch can trigger various cellular processes that may influence kidney function, either positively or negatively, depending on individual health factors.
Conflicting Claims: Does Intermittent Fasting Help or Harm Kidneys?

Potential positive and negative effects of intermittent fasting on kidney health
The scientific community remains divided on whether intermittent fasting benefits or harms kidney health. This division stems from conflicting research findings and the complex relationship between fasting, metabolism, and kidney function.
Potential Benefits for Kidney Health
- Reduced inflammation: Some studies suggest IF may decrease systemic inflammation, which could benefit kidney tissues
- Improved blood pressure: Better blood pressure control through IF may reduce strain on the kidneys
- Enhanced autophagy: Cellular cleanup processes activated during fasting might help remove damaged kidney cells
- Weight management: Weight loss from IF could reduce obesity-related kidney stress
- Better glycemic control: Improved insulin sensitivity may protect against diabetic kidney disease
Potential Risks for Kidney Health
- Dehydration: Extended fasting periods may increase dehydration risk, stressing the kidneys
- Electrolyte imbalances: Fasting can disrupt normal electrolyte levels, affecting kidney function
- Increased kidney stress: Some research suggests fasting might temporarily increase kidney workload
- Kidney stone risk: Potential increased risk of kidney stones due to concentrated urine during fasting
- Worsened kidney function: Some studies show fasting may worsen kidney function in those with existing CKD
Key Takeaway
The effects of intermittent fasting on kidney health likely depend on individual factors, including existing kidney function, hydration status, fasting duration, and underlying health conditions. What benefits one person may harm another.
A 2021 study published in the journal Kidney International found that intermittent fasting reduced albuminuria (protein in urine) in patients with type 2 diabetes and diabetic nephropathy. However, these benefits disappeared once participants returned to their normal eating patterns, suggesting that consistent fasting might be necessary for sustained kidney benefits.
Conversely, a 2017 study of 65 adults with stage 3 or higher CKD found that fasting during Ramadan was associated with worsened kidney function. Yet other studies have found no negative effects of similar fasting patterns on kidney health, highlighting the need for more research in this area.
How Intermittent Fasting Affects Kidney Function: 5 Key Mechanisms
Five key mechanisms through which intermittent fasting may influence kidney function
Understanding the biological mechanisms behind intermittent fasting’s effects on kidney function helps explain the conflicting research findings. Here are five key ways intermittent fasting might influence your kidneys:
1. Autophagy and Cellular Repair
Intermittent fasting triggers autophagy, a process where cells remove damaged components and regenerate healthier ones. In kidney cells, enhanced autophagy may help clear damaged proteins and organelles, potentially slowing kidney disease progression. A 2020 study published in Cell Metabolism demonstrated that fasting-induced autophagy reduced kidney damage in mouse models of polycystic kidney disease.
2. Blood Pressure Regulation
Hypertension is a leading cause of kidney damage. Intermittent fasting may help regulate blood pressure through weight loss, improved insulin sensitivity, and reduced inflammation. A 2023 systematic review in Nutrients found that various intermittent fasting protocols reduced systolic and diastolic blood pressure in most participants, which could indirectly benefit kidney health.
Relationship between fasting duration, blood pressure, and kidney function markers
3. Metabolic Pathway Alterations
During fasting, the body shifts from using glucose to ketones for energy. This metabolic switch affects various signalling pathways that influence kidney function. Research published in the Journal of Clinical Investigation suggests that ketone bodies produced during fasting may protect against acute kidney injury by reducing oxidative stress and inflammation in kidney tissues.
4. Electrolyte Balance and Hydration
Fasting periods can affect fluid and electrolyte balance, which directly impacts kidney workload. Without adequate hydration during eating windows, the kidneys must work harder to maintain proper electrolyte levels and filter more concentrated waste products. This increased workload could potentially stress the kidneys, especially in those with existing kidney issues.
5. Inflammation Reduction
Chronic inflammation contributes to kidney disease progression. Intermittent fasting has been shown to reduce inflammatory markers like C-reactive protein, TNF-alpha, and IL-6. A 2022 study in the American Journal of Physiology-Renal Physiology found that intermittent fasting reduced kidney inflammation in animal models of diabetic nephropathy.
“The metabolic changes induced by intermittent fasting appear to have both protective and potentially harmful effects on kidney function, depending on individual health status, hydration levels, and the specific fasting protocol used.”
— Dr. Mark Mattson, Neuroscientist and Intermittent Fasting Researcher
Recent Clinical Evidence: What Studies Show About IF and Kidney Biomarkers

Researchers analysing kidney function biomarkers in clinical studies
Recent clinical studies (2020-2024) have provided new insights into how intermittent fasting affects key kidney biomarkers. These biomarkers help assess kidney function and include measurements like creatinine levels, estimated glomerular filtration rate (egfr), and protein in urine (proteinuria).
| Study (Year) | Participants | Fasting Protocol | Duration | Key Findings on Kidney Biomarkers |
| Sulaj et al. (2021) | 40 adults with type 2 diabetes and diabetic nephropathy | Fasting-mimicking diet (5 days/month) | 6 months | Reduced albuminuria, improved glycemic control, and better blood pressure regulation |
| Jiao et al. (2020) | 31 adults with CKD stages 2-4 | Time-restricted eating (10-hour window) | 12 weeks | No significant change in eGFR; reduced inflammatory markers |
| Nowak et al. (2022) | 28 adults with polycystic kidney disease | Alternate-day fasting | 3 months | Slowed cyst growth; stabilised egfr compared to the control group |
| Hassan et al. (2023) | 65 adults with stage 3 CKD | Ramadan-style fasting | 30 days | Mixed results: 40% showed worsened kidney function; 60% remained stable |
| Corley et al. (2024) | 52 adults with type 2 diabetes | 5:2 diet | 6 months | Improved creatinine clearance; reduced proteinuria in participants who lost >5% body weight |
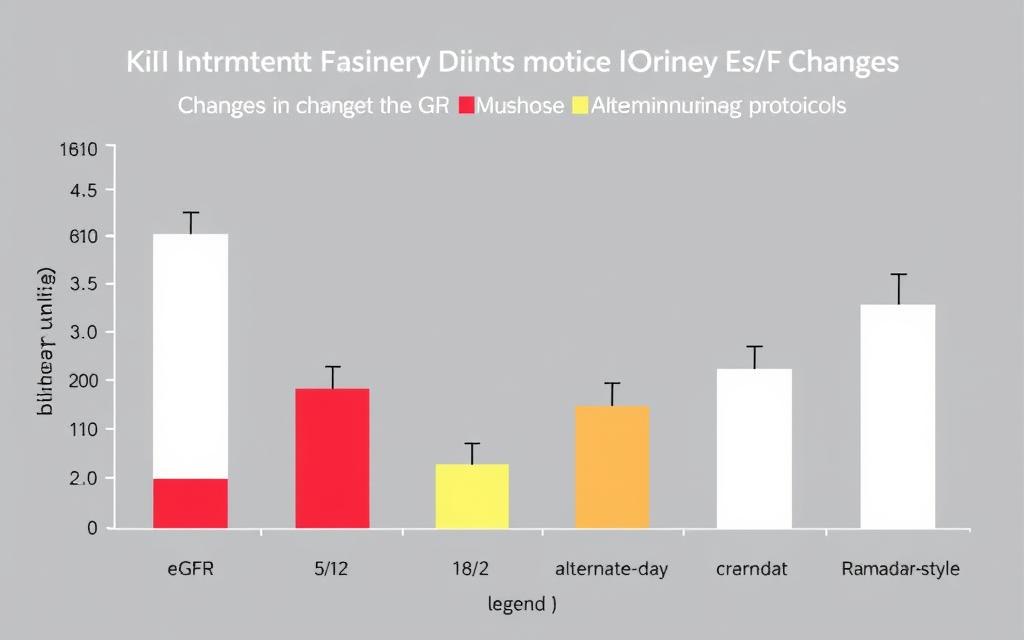
Changes in kidney function markers across different intermittent fasting protocols
Consensus Areas in Research
Despite some conflicting findings, researchers generally agree on several points:
- Short-term intermittent fasting (up to 16 hours) appears safe for individuals with normal kidney function
- Adequate hydration during eating windows is crucial for kidney protection during fasting
- Weight loss resulting from intermittent fasting may indirectly benefit kidney health
- Benefits appear most pronounced in those with metabolic conditions like diabetes and obesity
- Effects of fasting on kidney biomarkers often disappear when normal eating patterns resume
Unresolved Questions
Several important questions remain unanswered in the current research:
- Which intermittent fasting protocol is optimal for kidney health?
- How do individual factors like age, sex, and ethnicity influence kidney responses to fasting?
- What is the long-term impact (5+ years) of intermittent fasting on kidney function?
- Can intermittent fasting slow progression in those already diagnosed with kidney disease?
- How should medication schedules be adjusted during fasting periods for those with kidney conditions?
Research Limitations
Most studies on intermittent fasting and kidney health have been relatively short-term (under 1 year), have small sample sizes, and often lack diversity in participants. Additionally, many studies rely on animal models, which may not perfectly translate to human kidney physiology.
Practical Advice: Is Intermittent Fasting Right for Your Kidney Health?

Healthcare provider discussing personalised fasting approaches based on kidney health status
Whether intermittent fasting is appropriate for you depends largely on your current kidney health status, other medical conditions, and individual risk factors. Here’s actionable advice for different groups:
For People with Healthy Kidneys
- Start with shorter fasting periods (12-14 hours) before attempting longer fasts
- Maintain adequate hydration during eating windows
- Monitor for symptoms like excessive fatigue, dizziness, or changes in urination
- Consider regular kidney function tests if practising intermittent fasting long-term
- Focus on nutrient-dense foods during eating windows to support kidney health

Maintaining hydration and preparing kidney-supportive foods during eating windows
For People with Chronic Kidney Disease (CKD)
Important: If you have CKD, consult with your nephrologist before attempting any form of intermittent fasting. The recommendations below should only be considered with medical supervision.
- CKD stages 1-2 with stable function: May consider gentle time-restricted eating (10-12 hour eating window) with close monitoring
- CKD stages 3-5: Generally advised against longer fasting periods; focus on consistent meal timing and kidney-friendly nutrition
- Transplant recipients: Typically should avoid intermittent fasting due to medication timing requirements
- Dialysis patients: Should not practice intermittent fasting without specific medical guidance
For People with Diabetes
Diabetes is a leading cause of kidney disease, making this group particularly important to address:
- Work closely with your healthcare provider to adjust medication timing and dosages
- Monitor blood glucose more frequently when fasting
- Consider shorter fasting windows (12-14 hours) to start
- Be alert for hypoglycemia symptoms, which can be more common during fasting
- Regular kidney function tests are especially important for this group
For People with Hypertension
High blood pressure is another major risk factor for kidney disease:
- Monitor blood pressure regularly when practising intermittent fasting
- Maintain consistent medication schedules, which may require adjusting fasting windows
- Focus on sodium reduction during eating periods
- Consider the 16/8 method, which has shown blood pressure benefits in some studies
Regular monitoring of blood pressure and other health markers is essential when fasting with kidney concerns
Safe Fasting Practices for Kidney Health
Regardless of your kidney health status, these practices can help minimise risks:
- Hydration: Drink 6-8 glasses of water during eating windows
- Electrolyte balance: Include potassium, magnesium, and sodium-containing foods as appropriate for your condition
- Gradual approach: Extend fasting periods gradually rather than jumping into extended fasts
- Quality nutrition: Focus on nutrient-dense, kidney-friendly foods during eating windows
- Regular monitoring: Track kidney function biomarkers if practising intermittent fasting long-term
How should I adjust my medication schedule during intermittent fasting?
Medication timing can be critical, especially for kidney patients. Work with your healthcare provider to determine if medications need to be taken with food and how to adjust your fasting schedule accordingly. Never change medication timing without medical guidance.
What symptoms indicate I should stop fasting immediately?
Stop fasting and seek medical attention if you experience severe headaches, dizziness, confusion, rapid heart rate, extreme fatigue, changes in urination patterns, or unusual swelling. These could indicate kidney stress or other serious issues.
Conclusion: Balancing the Evidence on Intermittent Fasting and Kidney Health
Weighing the benefits and risks of intermittent fasting for kidney health
The relationship between intermittent fasting and kidney health is nuanced and highly individualised. Current research suggests that while intermittent fasting may offer benefits for some people, particularly those with obesity, diabetes, or early-stage kidney issues, it may pose risks for others, especially those with advanced kidney disease or specific medical conditions.
Key Takeaways
- Intermittent fasting affects kidney function through multiple mechanisms, including autophagy, metabolic shifts, and changes in blood pressure
- Benefits appear most consistent for those with metabolic conditions that put the kidneys at risk
- Risks increase with more advanced kidney disease, longer fasting periods, and inadequate hydration
- Individual responses vary significantly based on existing kidney function, age, and other health factors
- Medical supervision is essential for anyone with existing kidney concerns
As research continues to evolve, our understanding of how intermittent fasting affects kidney health will become clearer. For now, a cautious, personalised approach under appropriate medical guidance represents the most prudent path forward.
Remember that intermittent fasting is just one potential tool in a comprehensive approach to kidney health. Other factors—including overall diet quality, physical activity, blood pressure management, and medication adherence—remain foundational to protecting your kidneys over the long term.
Always consult with your healthcare provider before starting any fasting regimen, especially if you have existing kidney concerns or conditions that affect kidney function. Your provider can help you weigh the potential benefits against the risks based on your specific health profile.
Stay Updated on Kidney Health Research
Get the latest findings on intermittent fasting and kidney health delivered to your inbox. Our newsletter provides evidence-based updates on kidney-protective strategies.
Free Guide: Safe Intermittent Fasting Protocols for Kidney Health
Download our comprehensive guide with customised fasting protocols based on your kidney health status, hydration strategies, and kidney-friendly meal plans for your eating windows.







